Designing Safer Healthcare Systems by Bridging Lived Experience and Systems Engineering
Healthcare SYSTEMS ARCHITECT
STRUCTURAL INVISIBILITY
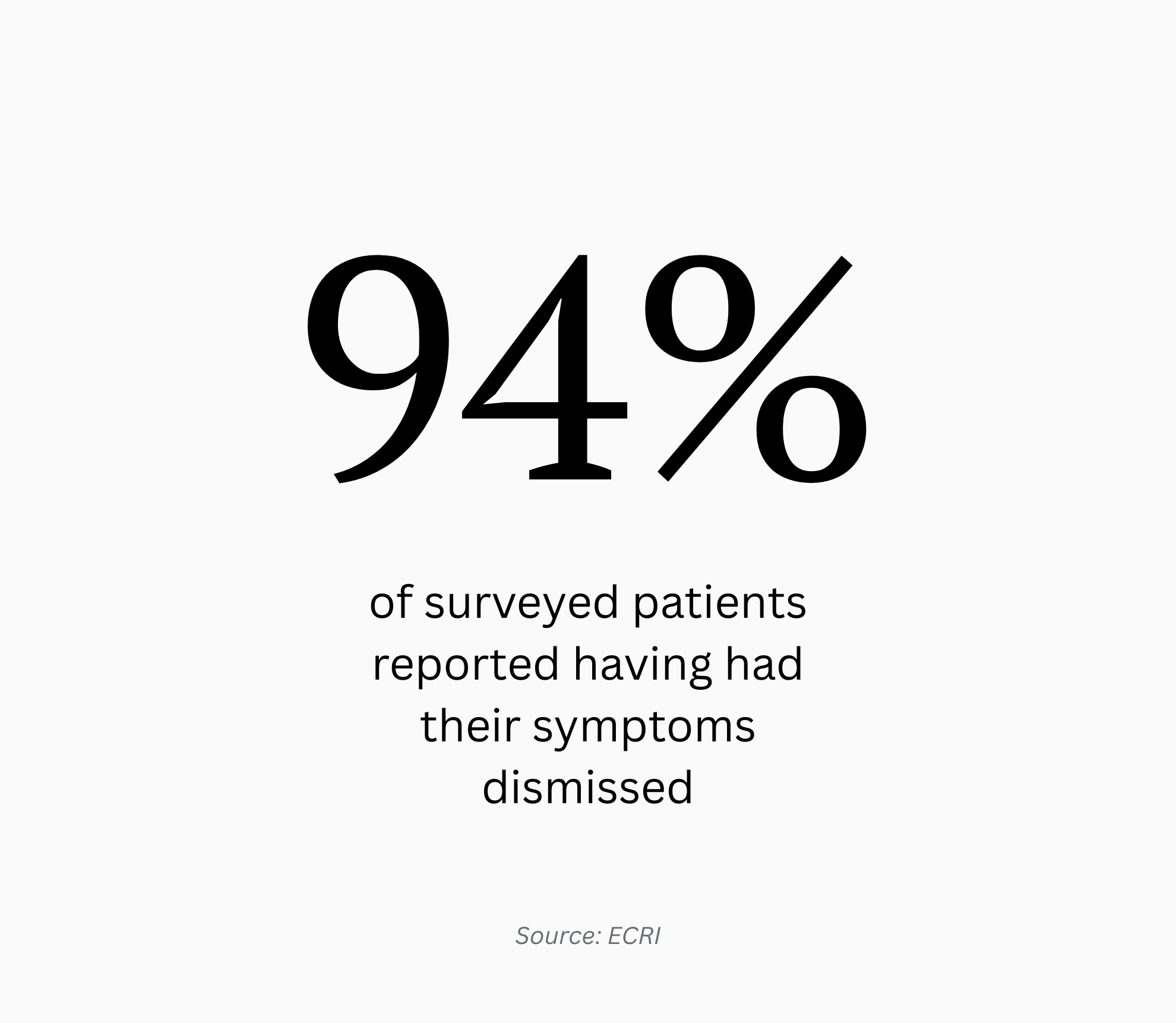
Healthcare systems can perform well by institutional measures while patients experience dismissal of their symptoms or diminished safety, revealing systemic risks that remain structurally unseen. In 2025, ECRI identified the “Risks of Dismissing Patient, Family, and Caregiver Concerns” as the top patient safety issue in the United States, underscoring the widespread nature of these structural gaps and the risks embedded within them. Yet they are often treated as individual provider lapses rather than recurring patterns of institutional risk. My work examines the blind spots that allow this dynamic to persist and why they matter for how healthcare systems perceive and manage risk, safety, and equity.
EXPOSED TO CARE
My work draws on decades of experience in systems engineering and design, alongside lived experience navigating healthcare as a cancer patient. I examine healthcare not as a series of clinical encounters, but as an engineered environment shaped by accumulated design decisions, incentives, and structural constraints. Holding these perspectives together—the architecture of the system and the reality of the patient—creates a dual vantage point that reveals risks neither institutional metrics nor patient advocacy alone can reliably surface.
RESEARCH & EDUCATION
I converted my experience inside healthcare into externally funded research, securing $1.75 million in innovation grant support from Genentech to examine structural blind spots in patient experience. In collaboration with Emory School of Medicine, I led multi-year research that resulted in the development of an educational program translating lived experience into system-level insight for clinicians and frontline healthcare leaders. I currently serve as faculty with the Medical Education Speakers Network, where I teach this work nationally. My research and analysis have appeared in STAT, the Journal of Patient Experience, Emory Medicine Magazine, and The Boston Globe.
CLINICAL RESONANCE
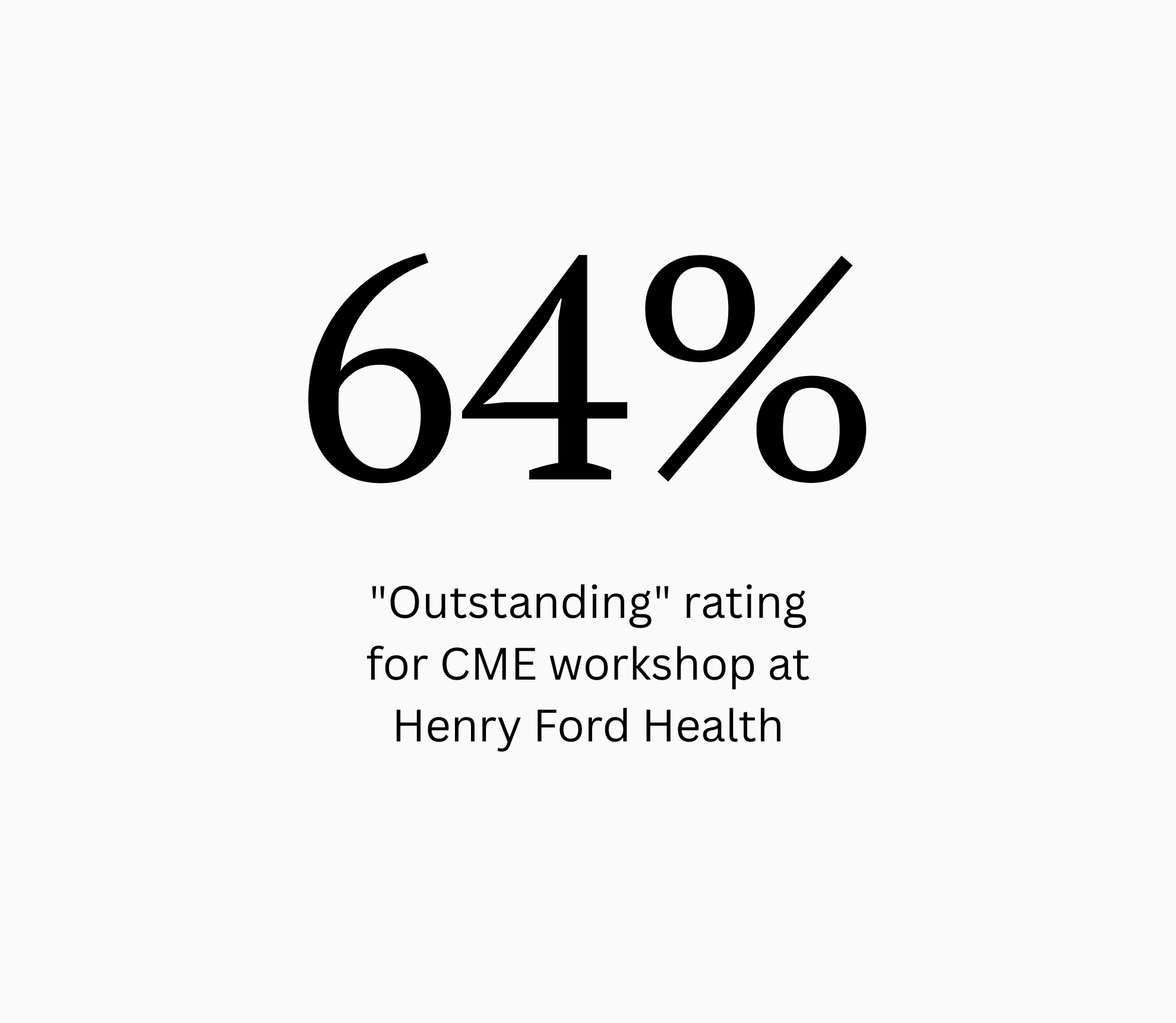
My presentations consistently receive high ratings from clinicians. At Henry Ford Health, 64% of participants rated my CME workshop on symptom dismissal as "Outstanding", with 96% citing it as directly relevant to their practice.
This feedback confirms that new approaches in medical education can make a traditionally fraught topic not only discussible, but also deeply engaging—turning what is often avoided or structurally invisible into a visible clinical priority.